引言
慢性阻塞性肺疾病(Chronic Obstructive Pulmonary Disease,COPD)是全球第四大主要死因[1],COPD急性加重(Acute Exacerbation of Chronic Obstructive Pulmonary Disease,AECOPD)是COPD自然病程中的重要不良事件[2].据统计,AECOPD具有相当高的住院率(24%)和1年死亡率(59%)[3],给全球医疗和经济系统带来巨大负担.AECOPD患者通常表现出呼吸困难、咳嗽及咳痰症状加重,症状往往不典型,且常伴有多种其他疾病,如心脏衰竭、肺炎和肺栓塞等,这增加了临床早期准确诊断的复杂性,可能延误最佳治疗时机[4].此外,药物治疗通常只能延缓疾病进展而无法治愈,早期诊断对于患者的治疗效果至关重要.
目前临床上对AECOPD的早期诊断主要依赖于肺功能检测(Pulmonary Function Tests,PFTs)和计算机断层扫描(Computed Tomography,CT).然而,考虑到COPD在急性加重期的病理特点涉及肺气肿和肺部微循环的变化等因素[5],PFTs虽可评估全局的气流阻塞,但对局部的通气功能不够敏感.而胸部CT扫描能够揭示肺部精细结构,定量评估肺气肿程度和气道壁变化,但难以对肺通气和气体交换功能的病变进行评估,且CT的辐射性限制了短期内的反复检查.因此亟需发展灵敏且安全的量化手段,以综合分析患者的病情,提高早期诊断和治疗的准确性和时效性.
超极化129Xe气体磁共振成像(Magnetic Resonance Imaging,MRI)是一项很有前景的技术,可用于观察和量化肺部的局部通气和气体交换功能[6⇓-8].这种功能性肺部MRI技术可以为CT提供信息补充,且由于其不具有电离辐射,因此可以作为纵向监测的一种手段.目前,超极化129Xe MRI已广泛应用于多种肺部疾病的诊疗评估,包括COPD、放射性肺损伤以及特发性肺纤维化等[9,10].超极化129Xe扩散加权成像(Diffusion Weight Imaging,DWI)测量的表观扩散系数(Apparent Diffusion Coefficient,ADC)、肺泡平均线性截距(Mean Linear Intercept,Lm)与组织学测量的末梢气道和肺泡的扩大程度相关[11⇓-13].大量的研究表明,超极化129Xe DWI能够有效检测COPD患者的肺部微结构病变[14,15].此外,气态129Xe进入肺泡后,能够穿过肺组织间隔进入肺毛细血管.由于129Xe具有良好的组织溶解性和化学位移敏感性,在肺部会产生3个不同化学位移的信号[16],分别为气态129Xe信号(Gas@0 ppm)、溶解在组织血浆中的129Xe信号(Tissue/Plasma,TP@197 ppm),溶解在红细胞内的129Xe信号(Red Blood Cell,RBC@217 ppm).这3种信号在肺内保持动态平衡,通过化学位移饱和恢复(Chemical Shift Saturation Recovery,CSSR)技术结合相关数据模型可以获得肺泡-毛细血管界面处的气血交换功能参数[17],如肺泡间隔壁厚度(肺组织与毛细血管内的血浆以及血红细胞被统一视为“肺泡间隔”)、肺泡表面体积比(单位肺体积的肺表面积)等,实现肺部气血交换功能的定量评估[18].
有研究指出,COPD患者接受支气管扩张剂治疗后尽管通气情况有所改善,但新通气区域仍存在129Xe的RBC转移缺陷[19].值得注意的是,这一发现并未在常规PFTs中探测到.另一研究发现,与非吸烟者相比,恶化的COPD患者的129Xe通气缺陷百分比的变化显著增高,并且基线通气缺陷百分比可以预测圣乔治呼吸问卷的纵向变化,但这一纵向变化尚未在CT中发现[20].研究还发现,基于129Xe MRI测量的肺叶平均ADC与肺叶定量CT肺气肿指标相关,全肺平均ADC与PFTs结果有中度相关性[21].此外,Qing等人的研究表明,相比健康志愿者,CSSR方法能够明显发现COPD患者的RBC/TP降低,同时肺泡间隔壁厚度升高[22].Stewart等人还发现,CSSR方法对肺泡间隔壁厚度的测量具有可重复性,并且随着肺部膨胀程度的增加,该方法测量的肺泡的表面积与体积比呈现下降趋势[23].基于这些研究,我们认为具备高灵敏度的超极化129Xe磁共振技术有望应用于AECOPD的早期诊断以及实现对AECOPD的风险预测,从而改善AECOPD患者的生活质量并降低死亡率.
肺气肿是COPD的重要疾病特征,肺气肿模型是COPD常用模型,本研究在肺气肿的基础上建立了AECOPD大鼠模型,采用超极化129Xe的DWI和CSSR方法,对该模型的肺部结构和功能变化进行检测,并将其结果与组织学检查以及肺功能测试进行对比,从而验证这一方法在评估AECOPD大鼠模型的可行性.
1 实验部分
1.1 动物准备
动物实验按照中国科学院精密测量科学与技术创新研究院机构动物伦理审查委员会提供并批准的指南进行.18只Wistar大鼠(体重180±10 g)被随机分成三组,对照组(NS组)、肺气肿组(PPE组)、肺气肿急性加重组(AE组).PPE组和AE组大鼠通过型号为14 G的经口气管插管,向气管内滴注猪胰腺弹性蛋白酶(Porcine Pancreatic Elastase,PPE;Elastin Products Company,USA)溶液,剂量为70 IU/100 g体重.NS组以同样的方式滴注等量的生理盐水.滴注完后,轻轻旋转大鼠身体,使药物在肺内分布均匀. 滴注完后监测老鼠的呼吸和行为,未发现不良反应.所有大鼠继续在SPF动物房正常饲养6周,然后向AE组的大鼠气管内滴注脂多糖(Lipopolysaccharide,LPS;O55:B5,SIGMA)溶液0.2 mL,药物浓度为 1 mg/mL,PPE组和NS组给予等量的生理盐水.滴注LPS或生理盐水24 h后,使用腹腔注射2%戊巴比妥钠溶液对大鼠进行麻醉并进行气管插管手术,然后依次进行PFTs,肺部超极化129Xe MRI以及肺组织提取和固定.
1.2 超极化129Xe气体的制备
基于自旋交换光抽运(Spin-Exchange Optical Pumping,SEOP)技术,使用商用的超极化气体发生器(verImagin Healthcare,中国)对129Xe气体进行超极化[24],所用的气源是2%同位素富集氙(129Xe富集度是86%)、88% 4He和10% N2的混合气体.超极化后的129Xe首先在液氮和磁场包围的冷阱内进行冷冻储存.每只大鼠需要180 mL气体,气体收集完后将Tedlar气体采样袋抽真空以去除其他残留气体,并将冷阱放入沸水浴中,将氙冰迅速升华到稳压罐内的Tedlar袋子中.
1.3 肺功能测试
PFTs在一台商用肺功能仪(CRFM 100,EMMS,UK)上进行,将气管插管后的大鼠连接到肺功能仪器上,大鼠首先进行2 min自由呼吸,以测量潮气量与呼吸频率,同时进行校准基线;随后依次测量大鼠的用力肺活量(FVC)、功能残气量(FRC)、200 ms以内的用力呼气量(Volume expired in first 200 ms of fast expiration,FEV200ms)和肺总量(TLC).上述所有参数均进行3次重复测量.
1.4 超极化129Xe MR扫描
完成PFTs实验后,将大鼠连接到超极化气体传输系统中.所有磁共振实验均在7.0 T动物扫描仪(Bruker BioSpec 70/20 USR,Germany)上进行.使用自制的收发一体式129Xe鸟笼线圈(共振频率83.07 MHz)进行信号的发射与接收.大鼠取仰卧位扫描,并使用超极化气体传输系统控制大鼠呼吸氧气和氙气.呼吸氧气时,吸气400 ms,呼气800 ms,潮气量2.0 mL.呼吸超极化氙气时,吸气500 ms,屏气时间1~5 s,呼气1 200 ms,潮气量2.5 mL,所有超极化129Xe MR数据获取均在该屏气时间内完成.实验期间,超极化气体传输系统持续监测肺内压力,且保持在0~15 cm H2O之间.
DWI:大鼠进行一次氙气预呼吸,随后再吸入一次氙气进行屏气采样.序列采集参数如下:梯度上升/下降沿时间=0.123 ms;梯度持续时间=1 ms;扩散时间=1.2 ms;回波时间(TE)/重复时间(TR)=4.11/22.43 ms;成像矩阵=64×64;翻转角度=8˚;视野大小=5×5 cm2;带宽=50 kHz;层厚=4 cm,实验采集了9个b值(4~32 s/cm2)的图像,用于圆柱模型拟合来获得肺泡微结构参数.每一个b值的图像都在一次单独的屏气内采集,该屏气内采集3幅施加和不施加扩散梯度(即b=0、x、0 s/cm2)的图像,以尽可能降低肺内的T1弛豫与射频激发对不同图像信号的影响.
CSSR:大鼠进行两次氙气预呼吸,随后再吸入一次氙气进行屏气采样.采用两个持续时间分别为0.5 ms和0.3 ms的高斯脉冲来分别饱和和激发溶解态129Xe信号,这两个脉冲对气态129Xe分别产生0.05˚和0.13˚的偏共振激发.24个交换时间点依次为2、4、6、8、10、15、20、25、30、35、40、45、50、60、70、80、90、100、150、200、250、300、350、400 ms,采样带宽为25 kHz,采样点数1 024.每只大鼠的CSSR实验均重复5次.计算交换时间在100 ms下获得的129Xe在RBC、TP及肺泡内的信号,分别记作SRBC,STP及SGas.同时,用两两之间的信号比值,如SRBC/STP、SRBC/SGas和STP/SGas反映129Xe在RBC、TP和肺泡之间的交换效率.结合氙交换模型(Model of Xe Exchange,MOXE)模型[14],可得到肺部微观结构和功能变化的参数,如肺泡间隔壁的厚度(d)、气血交换膜厚度(Δ)、肺泡的表面积与体积比(SVR)、交换时间常数(T)、红细胞比容(HCT)和129Xe在RBC与血液中信号的比值(η)等参数.
1.5 组织学测量
超极化129Xe MR实验完成后,取出离体肺组织,通过插管向肺内滴入4%多聚甲醛溶液,并在25 cmH2O压力下固定48 h.之后使用石蜡进行包埋,然后在每个肺叶的最大截面方向切成5 μm厚的切片,并对切片进行苏木精和伊红(H&E)染色.利用相机(Nikon Eclipse Ts 100;Japan)对每张切片拍照.利用Image-Pro Plus软件(Media Cybernetics;Buckinghamshire,UK),在照片上绘制规则的网格,根据网格被肺泡所截断的长度计算肺泡平均线性截距Lm[25].
1.6 统计学方法
数据统计分析利用SPSS(IBM,Armonk,NY,USA)软件,采用单因素方差分析评估NS组、PPE组和AE组的PFTs、MR实验以及定量组织学得到的所有定量结果.使用Pearson方法探究了大鼠全肺ADC均值与组织学测量的Lm,DWI测量的Lm与组织学测量的Lm、CSSR获得的SRBC/STP与FRC以及SRBC/SGas与FRC之间的相关性.P < 0.05为差异有统计学意义.
2 结果与讨论
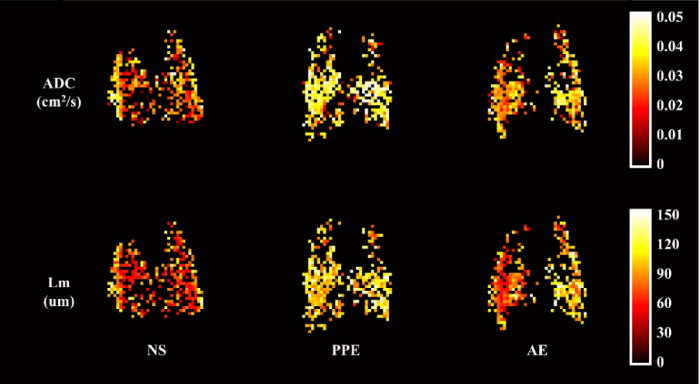
2.1 肺部微结构成像
图1展示了三组大鼠的代表性的DWI结果.第一行是ADC分布图,而第二行是Lm分布图.从左到右分别是NS组、PPE组和AE组.观察发现,相较于NS组,PPE组双肺均出现ADC和Lm升高;相较于PPE组,AE组右肺下叶、左肺上叶均表现出ADC和Lm的下降.
图1
表1统计了本次DWI实验测得的3组大鼠ADC、Lm和SVR的均值和标准差的测量结果.PPE组较NS组ADC显著增大(P<0.01).与PPE组相比,AE组ADC无显著变化,但仍高于NS组(P<0.05);PPE组和AE组的Lm、SVR较NS组均显著增大(PPE组:P<0.001,AE组:P<0.01),AE组与PPE组之间Lm、SVR无显著差异.
表1 超极化129Xe DWI测得的ADC、Lm和SVR平均值
Table 1
| 参数 | NS组 | PPE组 | AE组 | P值a | P值b | P值c |
|---|---|---|---|---|---|---|
| ADC/(cm2/s) | 0.028±0.001 | 0.033±0.003 | 0.032±0.002 | 0.0014 | 0.3540 | 0.0112 |
| Lm/μm | 85.71±4.94 | 101.11±6.59 | 98.77±7.94 | 0.0009 | 0.5314 | 0.0044 |
| SVR/cm-1 | 508.50±1.44 | 411.09±26.86 | 435.62±37.89 | 0.0001 | 0.1739 | 0.0010 |
a表示NS组、PPE组之间比较的P值,b表示PPE组、AE组之间比较的P值,c表示NS组、AE组之间比较的P值.
2.2 气血交换功能结果
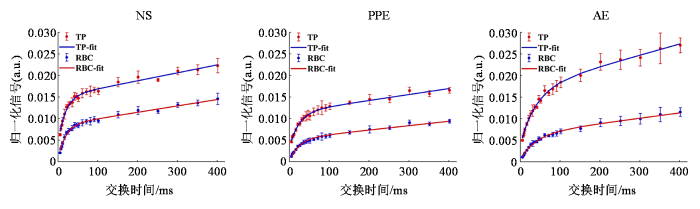
图2展示了溶解态129Xe信号建立曲线.与NS组相比,PPE组RBC和TP信号建立曲线明显降低;与PPE组相比,AE组的TP信号建立曲线升高.
图2
图2
溶解态129Xe信号的建立曲线
Fig. 2
Typical dissolved 129Xe signal build up curves for each group
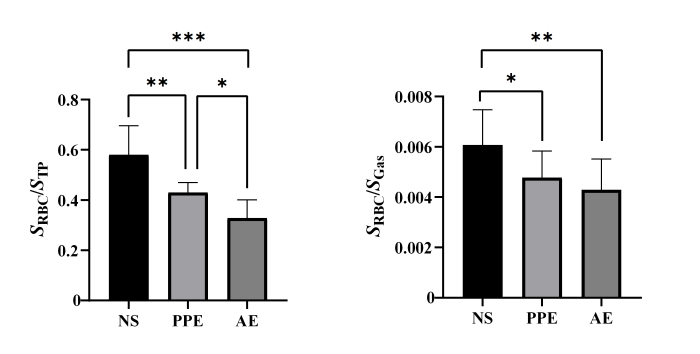
图3显示了NS组、PPE组以及AE组100 ms交换时间下的SRBC/STP、SRBC/SGas的变化,与NS相比,PPE组的SRBC/STP、SRBC/SGas显著下降(SRBC/STP:P<0.01,SRBC/SGas:P<0.05),AE组的SRBC/STP、SRBC/SGas显著下降(SRBC/STP:P<0.001,SRBC/SGas:P<0.01);与PPE组相比,AE组的SRBC/STP进一步下降(P<0.05).
图3
图3
三组大鼠的SRBC/STP和SRBC/SGas的比较,*代表P<0.05,**代表P<0.01,***代表P<0.001
Fig. 3
Comparison of the SRBC/STP and SRBC/SGas ratios among three groups, *P<0.05, **P<0.01, ***P<0.001
表2汇总了CSSR方法结合MOXE模型得到的肺部生理学参数,与NS组相比,PPE组的T、Δ/d、HCT、SVR、η无显著变化(P>0.05);相比于PPE组,AE组的Δ/d、η、HCT显著下降(P<0.01).
表2 结合MOXE模型所计算出的肺部生理学参数
Table 2
| 参数 | NS组 | PPE组 | AE组 | P值a | P值b | P值c |
|---|---|---|---|---|---|---|
| T/ms | 15.36±2.37 | 20.20±5.79 | 26.21±4.90 | 0.112 | 0.054 | 0.003 |
| d/μm | 7.06±1.22 | 8.04±1.13 | 9.21±0.88 | 0.095 | 0.055 | 0.002 |
| Δ/d | 0.149±0.038 | 0.180±0.033 | 0.122±0.018 | 0.129 | 0.009 | 0.193 |
| HCT | 0.335±0.051 | 0.298±0.014 | 0.189±0.030 | 0.102 | 0.001 | 0.001 |
| SVR/cm-1 | 219.36±38.64 | 187.56±19.87 | 181.78±35.12 | 0.119 | 0.767 | 0.082 |
| η | 0.511±0.057 | 0.470±0.016 | 0.326±0.047 | 0.132 | 0.001 | 0.001 |
a表示NS组、PPE组之间比较的P值,b表示PPE组、AE组之间比较的P值,c表示NS组、AE组之间比较的P值.
2.3 肺功能检查
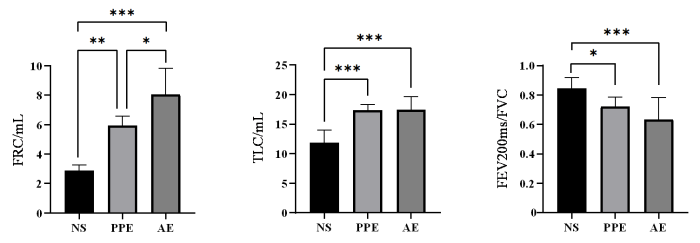
图4显示了小动物肺功能仪测量的NS组、PPE组、AE组的功能残气量FRC、肺总量TLC、 FEV200 ms/FVC的变化.与NS组相比,PPE组的FEV200 ms/FVC显著下降(P<0.05),FRC、TLC显著增大(FRC:P<0.01,TLC:P<0.001);与NS组相比,AE组的FEV200 ms/FVC显著下降(P<0.001),FRC、TLC显著增大(P<0.001);AE组的FRC较PPE组进一步显著增加(P<0.05).
图4
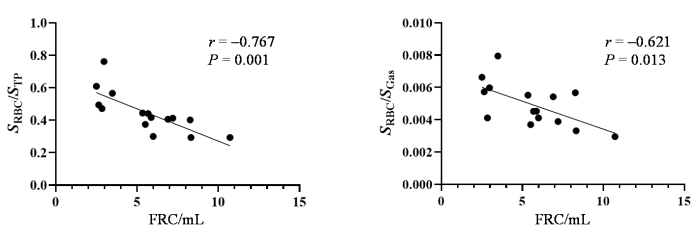
图5显示了三组大鼠CSSR测得的SRBC/STP(100 ms)、SRBC/SGas(100 ms)与FRC的相关性. SRBC/STP(100 ms)与FRC的相关性:r = -0.767,P = 0.001,为强相关;SRBC/SGas(100 ms)与FRC的相关性:r = -0.621,P < 0.05,为中等程度相关.
图5
图5
SRBC/STP和SRBC/SGas分别与FRC的相关性
Fig. 5
Correlations of SRBC/STP and SRBC/SGas with FRC, respectively
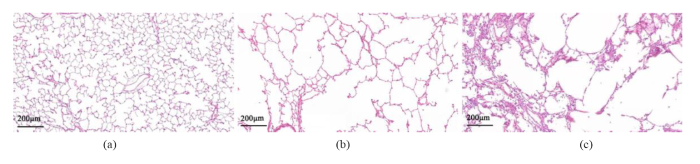
2.4 病理组织学结果
图6展示了NS组、PPE组、以及AE组大鼠的苏木精和伊红(H&E)染色肺组织切片.与NS组相比,PPE组均表现出全肺的肺泡腔的增大,AE组大鼠除肺泡明显增大外,肺泡间隔及肺泡内可见大量的炎症细胞浸润.用image-pro plus软件对三组大鼠的病理切片平均肺泡大小进行了测量.与NS组大鼠的Lm(82.81±1.50 μm)相比,PPE组的大鼠Lm(125.01±7.03 μm)显著增大(P<0.0001),增加了约50%.与PPE组相比,AE组的Lm(119.14±3.93 μm)轻度下降,但无显著统计学差异.
图6
图6
NS组(a)、PPE组(b)和AE组(c)的代表性肺部病理切片
Fig. 6
Representative lung pathological sections from (a) control group, (b) emphysema group and (c) acute exacerbation group
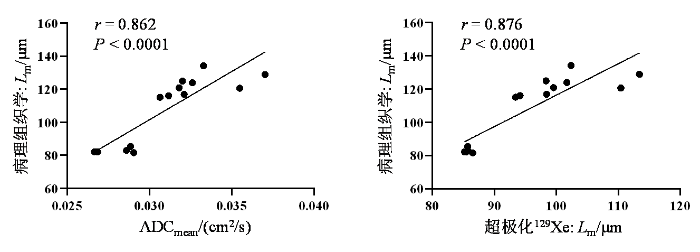
图7显示了三组大鼠DWI测量的全肺ADC均值(ADCmean)以及结合圆柱模型所计算出的Lm与病理组织学测量的Lm的相关性;ADC与组织病理学对的Lm的相关性:r = 0.862,P < 0.0001;DWI计算出的Lm与组织病理学的Lm的相关性:r = 0.876,P < 0.0001.
图7
图7
超极化129Xe ADCmean、Lm分别与病理组织学测得的Lm之间的关系
Fig. 7
Correlations between ADCmean, Lm obtained with hyperpolarized 129Xe MRI and Lm obtained with histology, respectively
3 讨论
超极化129Xe DWI检测到PPE组和AE组ADC以及Lm的全肺均值显著增大,且具有更大的标准差.这种肺气肿程度的差异可能与大鼠个体差异或者肺内药物分布不均匀有关.然而,没有发现AE组较PPE组的肺泡进一步扩张,这可能是由于该疾病模型短期肺内大量炎症细胞的浸润,以及粘液分泌增多所致.在DE OLIVEIRA等人[27]的研究中,急性加重24 h后,Lm出现了显著下降,或Lm的增大[28].Lm的变化可能受到肺气肿的程度以及滴注LPS后的检测时间点影响.CSSR结果显示,相比于NS组,PPE组的SRBC/STP、SRBC/SGas显著下降,说明肺组织弹性纤维等结构的长期破坏导致了肺部气血交换功能的下降;相比于PPE组,AE组的SRBC/STP进一步显著下降,红细胞比容HCT以及气血交换膜与肺泡间隔壁厚度的比值显著下降,可能是炎症进一步导致肺泡腔的阻塞以及膈肌的耐力下降,加剧了气血交换功能的恶化.SVR与肺泡结构的破坏有关,该研究中通过CSSR方法和DWI中测得各组之间的SVR值变化不一致,DWI中测得AE组和PPE组的SVR值较NS组显著下降,符合肺气肿的特征,并且数值与Zhang等人[29]测得的数值相近,而CSSR中测得的SVR各组之间无显著变化,这可能是CSSR方法对于该结构参数的测量误差所致.PFTs发现PPE组大鼠TLC的增大,FRC的增加以及FEV200ms/FVC的下降,AE组进一步表现出FRC的显著增加.急性加重后,与人类COPD疾病诊断标准FEV1/FVC所对应的FEV200ms/FVC并未表现出显著变化.这些结果说明在评估该疾病模型时,CSSR获得的参数比PFTs获得的参数更加敏感.病理组织学分析发现,PPE组与AE组均表现出明显的肺泡融合破裂,肺泡腔增大,而AE组进一步表现出炎症细胞浸润,肺泡间隔增厚等改变.
本研究初步验证了超极化129Xe MR评估AECOPD的肺部微结构和功能的可行性,有望将该项技术用于COPD人群加重风险的预测.但该研究也存在一些限制因素:第一,DWI测量肺部的微观结构是基于简化的圆柱模型,而实际的肺泡微观结构比所用的模型要复杂得多. DWI中测得的Lm是冠状面投影的平均大小,并未对前胸到后背方向的Lm异质性进行评估.因此,在以后的研究中,建立更接近肺部微结构的模型以及发展各向同性分辨的DWI方法仍需要探索.除此之外,局部肺区域与病理组织学之间的对比研究也需要开展,从而确定该方法对局部病灶评估的准确性.第二,疾病动物模型往往不能完全符合人类COPD疾病特征,该AECOPD模型是在肺气肿模型构建基础上进行,加重后肺泡结构和气血交换功能的变化受到肺气肿基础模型轻重程度以及肺气肿分布均匀程度的影响,引起炎症损伤的LPS的剂量和作用时间也会影响到疾病的加重过程,进而影响疾病模型的特征;第三,我们尚未量化炎症细胞在AECOPD中的作用,从而难以界定超极化129Xe MR对急性加重程度评估的灵敏度;第四,本研究只对急性加重24 h后进行了检测,而感染对肺气肿人群的持续性影响和生理机制还有待探究.目前基于超极化129Xe MR的AECOPD的研究才刚刚起步,许多相关方面的理论和实验研究仍需要进一步探索和完善.
4 结论
本研究利用气管内滴注弹性蛋白酶获得肺气肿模型,通过继续滴注LPS引起急性炎症变化,从而成功构建了AECOPD模型,并使用超极化129Xe MR对该模型肺泡微结构和气血交换功能的改变进行了定量评估.结果发现,肺气肿模型的平均肺泡大小显著增大,急性加重后其气血交换功能在短期内显著下降.这些发现与在组织学检查和肺功能检查的结果具有较好的一致性,证明了使用该方法评估肺气肿模型急性加重后的微观结构和气血交换功能变化的可行性和有效性.不仅为COPD患者合并炎症感染急性加重后的肺部功能变化的评估提供了新的思路,也对临床中AECOPD疾病的辅助诊断、更早期发现COPD的急性加重以及更全面准确的评估疾病加重程度具有积极的作用.
利益冲突
无
参考文献
Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the global burden of disease study 2015
[J].
DOI:10.1016/S2213-2600(17)30293-X
PMID:28822787
[本文引用: 1]

Chronic obstructive pulmonary disease (COPD) and asthma are common diseases with a heterogeneous distribution worldwide. Here, we present methods and disease and risk estimates for COPD and asthma from the Global Burden of Diseases, Injuries, and Risk Factors (GBD) 2015 study. The GBD study provides annual updates on estimates of deaths, prevalence, and disability-adjusted life years (DALYs), a summary measure of fatal and non-fatal disease outcomes, for over 300 diseases and injuries, for 188 countries from 1990 to the most recent year.We estimated numbers of deaths due to COPD and asthma using the GBD Cause of Death Ensemble modelling (CODEm) tool. First, we analysed data from vital registration and verbal autopsy for the aggregate category of all chronic respiratory diseases. Subsequently, models were run for asthma and COPD relying on covariates to predict rates in countries that have incomplete or no vital registration data. Disease estimates for COPD and asthma were based on systematic reviews of published papers, unpublished reports, surveys, and health service encounter data from the USA. We used the Global Initiative of Chronic Obstructive Lung Disease spirometry-based definition as the reference for COPD and a reported diagnosis of asthma with current wheeze as the definition of asthma. We used a Bayesian meta-regression tool, DisMod-MR 2.1, to derive estimates of prevalence and incidence. We estimated population-attributable fractions for risk factors for COPD and asthma from exposure data, relative risks, and a theoretical minimum exposure level. Results were stratified by Socio-demographic Index (SDI), a composite measure of income per capita, mean years of education over the age of 15 years, and total fertility rate.In 2015, 3·2 million people (95% uncertainty interval [UI] 3·1 million to 3·3 million) died from COPD worldwide, an increase of 11·6% (95% UI 5·3 to 19·8) compared with 1990. There was a decrease in age-standardised death rate of 41·9% (37·7 to 45·1) but this was counteracted by population growth and ageing of the global population. From 1990 to 2015, the prevalence of COPD increased by 44·2% (41·7 to 46·6), whereas age-standardised prevalence decreased by 14·7% (13·5 to 15·9). In 2015, 0·40 million people (0·36 million to 0·44 million) died from asthma, a decrease of 26·7% (-7·2 to 43·7) from 1990, and the age-standardised death rate decreased by 58·8% (39·0 to 69·0). The prevalence of asthma increased by 12·6% (9·0 to 16·4), whereas the age-standardised prevalence decreased by 17·7% (15·1 to 19·9). Age-standardised DALY rates due to COPD increased until the middle range of the SDI before reducing sharply. Age-standardised DALY rates due to asthma in both sexes decreased monotonically with rising SDI. The relation between with SDI and DALY rates due to asthma was attributed to variation in years of life lost (YLLs), whereas DALY rates due to COPD varied similarly for YLLs and years lived with disability across the SDI continuum. Smoking and ambient particulate matter were the main risk factors for COPD followed by household air pollution, occupational particulates, ozone, and secondhand smoke. Together, these risks explained 73·3% (95% UI 65·8 to 80·1) of DALYs due to COPD. Smoking and occupational asthmagens were the only risks quantified for asthma in GBD, accounting for 16·5% (14·6 to 18·7) of DALYs due to asthma.Asthma was the most prevalent chronic respiratory disease worldwide in 2015, with twice the number of cases of COPD. Deaths from COPD were eight times more common than deaths from asthma. In 2015, COPD caused 2·6% of global DALYs and asthma 1·1% of global DALYs. Although there are laudable international collaborative efforts to make surveys of asthma and COPD more comparable, no consensus exists on case definitions and how to measure disease severity for population health measurements like GBD. Comparisons between countries and over time are important, as much of the chronic respiratory burden is either preventable or treatable with affordable interventions.Bill & Melinda Gates Foundation.Copyright © 2017 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license. Published by Elsevier Ltd.. All rights reserved.
Epidemiology and prevalence of chronic obstructive pulmonary disease
[J].
Ultrasound-assessed diaphragmatic impairment is a predictor of outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease undergoing noninvasive ventilation
[J].
Thoracic imaging at exacerbation of chronic obstructive pulmonary disease: a systematic review
[J].
MRI-assessed diaphragmatic function can predict frequent acute exacerbation of COPD: a prospective observational study based on telehealth-based monitoring system
[J].
DOI:10.1186/s12890-022-02254-x
PMID:36424599
[本文引用: 1]

Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) have considerably high mortality and re-hospitalisation rate. Diaphragmatic dysfunction (DD) is common in COPD patients. However, whether diaphragmatic dysfunction is related to acute exacerbation is yet to be elucidated. This study aimed to evaluate the diaphragm function by magnetic resonance imaging (MRI) in COPD patients and assess whether the impact of DD may help predict AECOPD.20 healthy adult volunteers and 80 COPD patients were enrolled. The diaphragms function parameters were accessed by MRI. Patients were guided to start self-management by the Telehealth-based monitoring system following the enrolment. Events of acute exacerbation of COPD were recorded by the system and confirmed by healthcare providers. Binary univariate and multivariate logistic regression analyses were performed to investigate the factors associated with the frequency of AECOPD. Receiver operating characteristic (ROC) curves were further used to assess the value of prediction indexes.Fifty-nine COPD patients completed a one-year follow-up based on the Telehealth-based monitoring system. The clinical outcomes showed that the diaphragm function parameters at the end of maximal breathing were lower in the COPD group than in the healthy control group (P < 0.05). ANOVA showed significant differences among Global Initiative for Chronic Obstructive Lung Disease (GOLD) stages for diaphragm function parameters, including chest wall motion, lung area, upper-lower diameter, and the diaphragm thickening fraction at the end of maximal breathing (P < 0.05). Moreover, significant differences in diaphragm function parameters were observed between patients with infrequent AECOPD (n = 28) and frequent AECOPD (n = 31) based on the frequency of AECOPD (P < 0.05). The diaphragm thickening fraction and the chest wall motion were associated with AECOPD after adjusting for age, sex, BMI, and lung functions, and the combination of predictions showed better accuracy in predicting the frequency of AECOPD.In COPD patients, diaphragm function parameters correlate with the severity of airflow limitation. The diaphragm thickening fraction and the chest wall motion were associated with the frequency of AECOPD and can predict it.© 2022. The Author(s).
Hyperpolarized gas magnetic resonance imaging of the lung
[J].
超极化气体肺部磁共振成像
[J].磁共振成像(MRI)技术具有非侵入、无放射性的特点,在临床疾病诊断中具有独特的优势,但是肺部空腔的特殊结构使传统质子MRI 无法对其直接成像.自旋交换光抽运(SEOP)方法可以使惰性气体原子的极化度增强4 个量级以上,从而使肺部的气体MRI 成为可能.该文介绍了超极化惰性气体肺部MRI 的最新研究进展,包括超极化气体磁共振相关参数的测量方法、肺部通气结构成像、肺部气体交换功能成像,同时比较了常用于肺部MRI气体的优点和缺点.
Quantitative evaluation of lung injury caused by PM2.5 using hyperpolarized gas magnetic resonance
[J].
Quantitative evaluation of pulmonary gas-exchange function using hyperpolarized 129Xe CEST MRS and MRI
[J].
3D Single-breath chemical shift imaging hyperpolarized 129Xe MRI of healthy, CF, IPF, and COPD subjects
[J].
Quantifying regional radiation-induced lung injury in patients using hyperpolarized 129Xe gas exchange magnetic resonance imaging
[J].
Measurement of 129Xe gas apparent diffusion coefficient anisotropy in an elastase-instilled rat model of emphysema
[J].
Evaluation of emphysema severity and progression in a rabbit model: comparison of hyperpolarized 3He and 129Xe diffusion MRI with lung morphometry
[J].
Detection of the mild emphysema by quantification of lung respiratory airways with hyperpolarized xenon diffusion MRI
[J].
DOI:10.1002/jmri.25408
PMID:27472552
[本文引用: 1]

To demonstrate the feasibility to quantify the lung respiratory airway in vivo with hyperpolarized xenon diffusion magnetic resonance imaging (MRI), which is able to detect mild emphysema in the rat model.The lung respiratory airways were quantified in vivo using hyperpolarized xenon diffusion MRI (7T) with eight b values (5, 10, 15, 20, 25, 30, 35, 40 s/cm ) in five control rats and five mild emphysematous rats, which were induced by elastase. The morphological results from histology were acquired and used for comparison.The parameters D (longitudinal diffusion coefficient), r (internal radius), h (alveolar sleeve depth), Lm (mean linear intercept), and S/V (surface area to lung volume ratio) derived from the hyperpolarized xenon diffusion MRI in the emphysematous group showed significant differences from those in the control group (P < 0.05). Additionally, these parameters correlated well with the Lm obtained by the traditional histological sections (Pearson's correlation coefficients >0.8).The lung respiratory airways can be quantified by hyperpolarized xenon diffusion MRI, showing the potential for mild emphysema diagnosis. Also, the study suggested that the hyperpolarized xenon D is more sensitive than D (transverse diffusion coefficient) to detect mild emphysema.1 J. Magn. Reson. Imaging 2017;45:879-888.© 2016 International Society for Magnetic Resonance in Medicine.
Comparison of 3He and 129Xe MRI for evaluation of lung microstructure and ventilation at 1.5 T
[J].
Diffusion-weighted hyperpolarized 129Xe MRI in healthy volunteers and subjects with chronic obstructive pulmonary disease
[J].
Temporal dynamics of hyperpolarized 129Xe resonances in living rats
[J].
MOXE: A model of gas exchange for hyperpolarized 129Xe magnetic resonance of the lung
[J].
Regional investigation of lung function and microstructure parameters by localized 129Xe chemical shift saturation recovery and dissolved-phase imaging: A reproducibility study
[J].
Regional gas exchange measured by 129Xe magnetic resonance imaging before and after combination bronchodilators treatment in chronic obstructive pulmonary disease
[J].
MRI ventilation abnormalities predict quality-of-life and lung function changes in mild-to-moderate COPD: longitudinal TINCan study
[J].
DOI:10.1136/thoraxjnl-2016-209770
PMID:28258250
[本文引用: 1]

: COPD biomarkers are urgently required for clinical trials of new therapies. We evaluated the longitudinal change and relationship of MRI and CT biomarkers of COPD with St. George's Respiratory Questionnaire (SGRO) and FEV worsening over 30 months. Among imaging biomarkers, only the longitudinal change in MRI ventilation defect percent (VDP) was greater in ever-smoker (n=34/p<0.05) and COPD (n=48/p<0.0001) subgroups compared with never-smokers (n=42). Only the longitudinal change in VDP was correlated with change in SGRQ (r=0.26/p=0.03), and only baseline VDP predicted longitudinal change in SGRQ>minimum clinically important difference (p=0.047) in mild-to-moderate COPD. These data strongly support the use of MRI intermediate endpoints in COPD studies.NCT02723474; Status: Recruiting.Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) please go to http://www.bmj.com/company/products-services/rights-and-licensing/.
Emphysema index based on hyperpolarized 3He or 129Xe diffusion MRI: performance and comparison with quantitative CT and pulmonary function tests
[J].
Assessment of lung function in asthma and COPD using hyperpolarized 129Xe chemical shift saturation recovery spectroscopy and dissolved-phase MRI
[J].
Reproducibility of quantitative indices of lung function and microstructure from 129Xe chemical shift saturation recovery (CSSR) MR spectroscopy
[J].
Study on the automatic accumulation-thawing device of hyperpolarized 129Xe
[J].
超极化129Xe自动收集-升华装置研究
[J].
DOI:10.11938/cjmr20222998
[本文引用: 1]

因其较高的核自旋极化度所提供的探测灵敏度,超极化<sup>129</sup>Xe气体已被成功应用于动物和人体磁共振成像(MRI).但是,在超极化<sup>129</sup>Xe的收集-升华过程中,多种因素会导致<sup>129</sup>Xe核自旋弛豫,进而限制其应用范围.本文通过理论模型分析和实验测量,验证了温度、磁场、螺旋冷阱材质等对冷冻恢复过程中超极化<sup>129</sup>Xe弛豫的影响;同时,测量了自动收集-升华装置的稳定性.研究结果表明,升华方式和冷阱材质对<sup>129</sup>Xe极化度损耗的影响显著;自制收集-升华装置的自动化程度高、长时间稳定,<sup>129</sup>Xe极化度的恢复率可达到85.6% ± 4.7%.本研究非常有助于提升超极化<sup>129</sup>Xe在动物和人体MRI中的使用效率.
Hyperpolarized 3He diffusion MRI and histology in pulmonary emphysema
[J].
Gallic acid suppresses inflammation and oxidative stress through modulating Nrf2-HO-1-NF-κB signaling pathways in elastase-induced emphysema in rats
[J].
Endotoxin-induced emphysema exacerbation: a novel model of chronic obstructive pulmonary disease exacerbations causing cardiopulmonary impairment and diaphragm dysfunction
[J].
DOI:10.3389/fphys.2019.00664
PMID:31191356
[本文引用: 2]

Chronic obstructive pulmonary disease (COPD) is a progressive disorder of the lung parenchyma which also involves extrapulmonary manifestations, such as cardiovascular impairment, diaphragm dysfunction, and frequent exacerbations. The development of animal models is important to elucidate the pathophysiology of COPD exacerbations and enable analysis of possible therapeutic approaches. We aimed to characterize a model of acute emphysema exacerbation and evaluate its consequences on the lung, heart, and diaphragm. Twenty-four Wistar rats were randomly assigned into one of two groups: control (C) or emphysema (ELA). In ELA group, animals received four intratracheal instillations of pancreatic porcine elastase (PPE) at 1-week intervals. The C group received saline under the same protocol. Five weeks after the last instillation, C and ELA animals received saline (SAL) or lipopolysaccharide (LPS) (200 μg in 200 μl) intratracheally. Twenty-four hours after saline or endotoxin administration, arterial blood gases, lung inflammation and morphometry, collagen fiber content, and lung mechanics were analyzed. Echocardiography, diaphragm ultrasonography (US), and computed tomography (CT) of the chest were done. ELA-LPS animals, compared to ELA-SAL, exhibited decreased arterial oxygenation; increases in alveolar collapse (< 0.0001), relative neutrophil counts ( = 0.007), levels of cytokine-induced neutrophil chemoattractant-1, interleukin (IL)-1β, tumor necrosis factor-α, IL-6, and vascular endothelial growth factor in lung tissue, collagen fiber deposition in alveolar septa, airways, and pulmonary vessel walls, and dynamic lung elastance (< 0.0001); reduced pulmonary acceleration time/ejection time ratio, (an indirect index of pulmonary arterial hypertension); decreased diaphragm thickening fraction and excursion; and areas of emphysema associated with heterogeneous alveolar opacities on chest CT. In conclusion, we developed a model of endotoxin-induced emphysema exacerbation that affected not only the lungs but also the heart and diaphragm, thus resembling several features of human disease. This model of emphysema should allow preclinical testing of novel therapies with potential for translation into clinical practice.
A single dose of lipopolysaccharide into mice with emphysema mimics human chronic obstructive pulmonary disease exacerbation as assessed by micro-computed tomography
[J].
Dynamic evaluation of acute lung injury using hyperpolarized 129Xe magnetic resonance
[J].
Functional and morphological assessment of early impairment of airway function in a rat model of emphysema
[J].
Hyperpolarized 3He ventilation defects used to predict pulmonary exacerbations in mild to moderate chronic obstructive pulmonary disease
[J].
The emerging clinical significance of the red cell distribution width as a biomarker in chronic obstructive pulmonary disease: a systematic review
[J].